Why Chronic Pain Requires More Than One Approach
Chronic pain is rarely the result of a single issue—and for that reason, it rarely responds to a single solution. Unlike acute pain, which is often short-lived and tied to a clear injury, chronic pain is complex, persistent, and influenced by multiple systems within the body and mind.
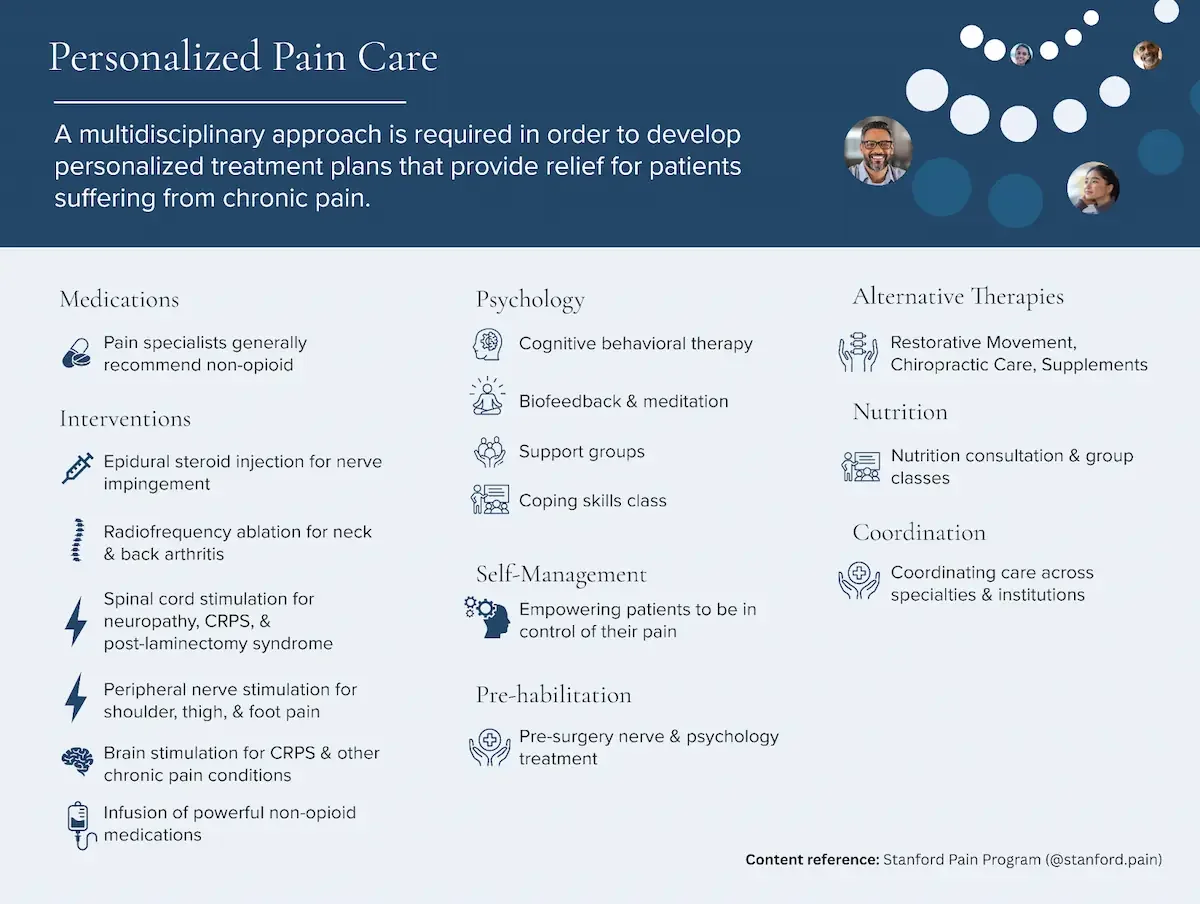
At Mind + Body Medicine in Dallas, we take a multidisciplinary approach to chronic pain care because experience—and research—continue to show that meaningful, lasting relief often requires more than one form of treatment working together.
Chronic Pain Is a Nervous System Condition, Not Just a Physical One
Over time, chronic pain can change how the nervous system functions. Pain signals may become amplified, pathways can remain active long after tissue healing has occurred, and the brain may begin to interpret normal sensations as threatening or painful.
Advanced diagnostic tools such as brain mapping allow clinicians to better understand how pain is being processed in the brain. When appropriate, therapies like brain stimulation may be used to help regulate abnormal neural activity and recalibrate pain signaling patterns—particularly in patients whose symptoms have not responded to conventional treatments alone.
Targeting Pain at the Source With Medical Therapies
Medical interventions remain an important component of comprehensive pain care, especially when pain involves nerve irritation, central sensitization, or inflammatory processes. Rather than relying on a single modality, treatment plans are designed to address pain at multiple levels.
For some patients, this may include infusion pain treatments that deliver non-opioid medications intravenously to reduce inflammation, calm the nervous system, and interrupt persistent pain cycles. Others may benefit from neuromodulation approaches such as magnetic peripheral nerve stimulation, which targets specific nerves involved in chronic pain without surgery or long recovery periods.
These therapies can significantly reduce pain intensity, but they are most effective when integrated into a broader, coordinated plan.
Addressing the Psychological and Emotional Dimensions of Pain
Chronic pain affects more than the body—it impacts mood, sleep, cognition, and emotional well-being. Anxiety, depression, and trauma can heighten pain perception, creating a feedback loop that reinforces symptoms over time.
In some cases, therapies such as ketamine-assisted psychotherapy may be incorporated to help patients process the emotional and neurological components of chronic pain. Unlike medication alone, this approach combines carefully administered ketamine with structured psychotherapy to address both the mental and physical dimensions of pain.
For patients who require neurochemical support without a psychotherapeutic component, ketamine infusion therapy may be used to help reset pain pathways and improve overall pain tolerance.
Empowering Patients Through Self-Management and Education
Long-term pain relief is rarely passive. Education, coping strategies, and self-management tools help patients regain a sense of control and reduce the day-to-day impact of chronic pain.
By understanding how stress, sleep, movement, and emotional health influence pain, patients are better equipped to manage flare-ups and participate actively in their care. This empowerment is a core component of multidisciplinary pain management and often plays a critical role in sustaining results over time.
Why Coordination Across Disciplines Matters
Perhaps the most important element of a multidisciplinary approach is coordination. Chronic pain is not static—it evolves, responds differently to treatment over time, and often requires adjustments along the way.
By integrating medical therapies, neurological interventions, psychological support, and patient education into a single, cohesive plan, care becomes more adaptive and responsive. Rather than treating symptoms in isolation, this model addresses the full spectrum of factors contributing to chronic pain.
A More Comprehensive Path Forward for Chronic Pain
Chronic pain is complex—but that complexity doesn’t mean relief is out of reach. It means patients deserve a care model that recognizes the interconnected nature of the body and mind.
Through advanced diagnostics, targeted therapies, psychological support, and coordinated care, a multidisciplinary approach offers a more complete and sustainable path forward—one designed to help patients move beyond symptom management and toward meaningful improvement in quality of life.
To learn whether a coordinated pain management plan may be right for you, schedule a consultation with Mind + Body Medicine in Dallas. Our team works collaboratively to develop individualized treatment strategies designed to address the full scope of chronic pain.